Ergocalciferol
By Jens Allmer
Ergocalciferol (vitamin D2) is made by plants and is similar to Cholecalciferol (vitamin D3), but it’s less effective for humans. D3 is better at raising vitamin D levels and has stronger effects in the body, while D2 binds less efficiently to the vitamin D receptors.
Studies have shown that D3 is more effective at improving vitamin D stores and lowering parathyroid hormone. Though some medications use high doses of D2, newer research suggests D3 supplements are a better choice. Plants like mushrooms and algae produce D2 when exposed to UVB light, but D2 levels are much lower than D3 found in fatty fish, for example.
In summary, D2 is similar to D3 but provides less bang for the buck.
For more technical details, read on.
Ergocalciferol (vitamin D2) is produced by plants. It resembles Cholecalciferol in animals but has a slightly different chemical structure. Notice the double-bond (two parallel lines) between carbon atoms 22 and 23 and the additional Carbon attached to position 24.
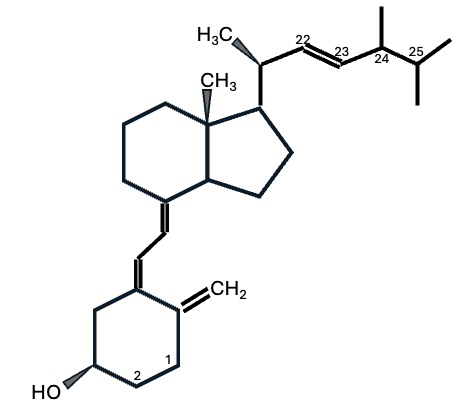 Chemical structure of Ergocalciferol
Chemical structure of Ergocalciferol
OK, there is a slight structural difference. What does that mean, though? Well, hormones are keys that fit certain locks, and vitamin D is actually a hormone. To perform its actions, many steps are necessary, including transport to the various places where the molecule is modified and finally binding to the vitamin D receptor (VDR, the lock) to convey function. Ergocalciferol is a foreign substance to the human body. There are three possibilities for substances that resemble hormones. 1) They bind less strongly to the receptors (the key doesn’t fit well), 2) they bind exactly like the original molecule, and 3) they bind stronger than the original molecule (the key fits even better).
Ergocalciferol falls into category 1. That means Ergocalciferol, if present in the same amounts as Cholecalciferol, is less efficiently transported, converted, and binds less efficiently to the final VDR receptor.
- Ergocalciferol is less bioavailable and has lower binding affinity than D3 versions of the molecule. Therefore, Houghton and Vieth (2006) recommend against It.
- Cholecalciferol is better at lowering parathyroid hormone and raising the Calcifediol stores (about twice as well) than Ergocalciferol (Romagnoli et al., 2008).
- Cholecalciferol led to a significantly higher increase in Calcifediol (the medium storage of D3) than Ergocalciferol (Glendenning et al., 2013).
- Many studies have shown that Cholecalciferol is more effective than acetate in resupplying the D3 stores in the blood (e.g., Wetmore et al., 2016; Mangoo-Karim et al., 2015).
If a foreign molecule binds better or worse, it can also cause side effects and diseases. Ergocalciferol seems relatively benign, and the pharmaceutical industry offers medications with high doses (50000 IU) of Ergocalciferol (D2). Examples of such drugs are Drisdol, Calciferol, Calcidiol, and Ergocal. These drugs have been around for a long time, and given the more recent research above, it is questionable whether Ergocalciferol should be used. At the same time, Cholecalciferol supplements with equally high doses exist so that there does not seem to be a need for drugs with high Ergocalciferol.
Plants only produce Ergocalciferol when exposed to UVB radiation. Interestingly, most species that are not strongly exposed to UVB contain Ergocalciferol.
- Mushrooms
- Yeast and Fungi
- Algae and Lichens
This means that the products must be irradiated with UVB artificially to produce Ergocalciferol. Still, the amount of Ergocalciferol doesn’t reach the Cholecalciferol levels present in fatty fish.
I think the case against Ergocalciferol supplementation is strong, but if you would like to read more about the plant version of vitamin D, ask below.
